Osteochondrosis is a widespread disease, at the age of 35-40 it is found in varying degrees in most people. The most likely localization of osteochondrosis is the lower cervical, upper thoracic and lower lumbar spine. The etiology of osteochondrosis, that is, the specific causes and conditions of its occurrence, is completely unknown. However, there is a direct influence of hereditary predisposition, age-related changes, injuries and impaired blood supply to tissues.
In the development of the disease, the main role is played by changes in the central part of the intervertebral disc, that is, dehydration. We recall that the disc consists of the nucleus pulposus and the annulus fibrosus around it. Due to drying, the disc loses its shock-absorbing functions, which leads to gradual destruction. In the development of the disease, four stages are distinguished, differing in certain changes in the disc and adjacent tissues. The severity of osteochondrosis of the spine, symptoms and treatment directly depend on the stage of development of the pathology.

Symptoms and causes of osteochondrosis of the spine
Let's briefly consider the stages of the progression of osteochondrosis in terms of anatomical changes.
- The first phase. The formation of cracks in the inner layers of the annulus fibrosus and in the nucleus pulposus. Penetrating into the cracks, the nucleus irritates the nerve endings of the fibrous ring;
- Second phase. As further irritation of the anulus fibrosus occurs due to the pathology of the nucleus pulposus, the fixation of the vertebrae deteriorates. There is unusual mobility of the spine;
- The third stage. Gradual damage to the annulus fibrosus. There is an extension of the nucleus (protrusion) beyond the anatomical limits of the fibrous annulus, and then there is rupture of the annulus and the formation of an intervertebral hernia (extrudion);
- The fourth stage. There is a spread of degenerative changes in the surrounding tissues - vertebrae, ligaments, nerves, blood vessels. As a result of chronic inflammation, the intervertebral disc is damaged, which leads to the development of fibrosis.
Depending on the location in the spine, there are 3 types of osteochondrosis:
- cervical osteochondrosis;
- thoracic osteochondrosis;
- Lumbar osteochondrosis.
It is worth noting that some sources distinguish the fourth type - sacral osteochondrosis.

Cervical osteochondrosis |
Thoracic osteochondrosis |
Lumbar osteochondrosis |
|---|---|---|
|
The main types of osteochondrosis are considered to be cervical and lumbar. However, the thoracic spine is under constant stress and is prone to the early development of severe degenerative changes, especially in young people. Due to the peculiarities of the development of changes in the thoracic spine, neurological symptoms appear at a late stage of the disease. In most cases, the disease appears with an injury (for example, as a result of excessive weight lifting).
|
Abnormalities are most often observed in the lumbar spine.
|

It was mentioned earlier that the etiology of osteochondrosis is not completely known. However, we can mention the main causes of osteochondrosis of the spine, with a proven effect on the development of the disease:
- Regular dynamic and static loads on the spine with different intensities. For example, the work of a loader (bearing weights) or a miner (being in unnatural positions for hours and a large physical load), a driver (vibration and a sedentary lifestyle) or an office worker (a sedentary lifestyle;
- back injury;
- Poor physical development or excess weight;
- Failure to maintain proper posture and bending;
- Flat feet and muscle imbalance as a result, leads to an uneven distribution of the load in different parts of the spine;
- genetic features;
- Hypothermia leads to more intense symptoms of osteochondrosis;
- And finally, the human aging process.
Diagnosis of osteochondrosis of the spine
The preliminary diagnosis of the disease (osteochondrosis) is made on the basis of the patient's complaints, his examination and palpation of the spine. Also, the affected part of the spine can be identified due to the topography of the pain distribution, which is able to show exactly where (in the vertebrae of the neck, chest, back) nerve compression has occurred.
The main diagnostic method for diagnosing osteochondrosis is X-ray examination. In the X-ray of the spine, degenerative changes in the intervertebral joints, discs, narrowing of the intervertebral canal, sclerotic changes in the tissues of the spine are observed. At the same time, recognizing lesions of the spine (especially at an early stage) is always difficult, since the processes occurring in this case are characteristic of a number of other diseases (tumors, metastases, ankylosing spondylitis, tuberculosis lesions).

In frontal x-ray images, the unevenness of the plates, an increase or sharpening of the uncinate processes is revealed. In profile images, a decrease in length, a change in shape, a disc herniation, osteophytes and other changes in the vertebral body are observed. Small degenerative changes are not visible on a plain radiograph, and an X-ray examination using contrast is performed to detect them. More complete information can be provided by discography - an X-ray examination with the introduction of a contrast agent through a puncture directly into the intervertebral disc.
Another study of the spine is a functional X-ray method. Thanks to the X-ray taken with maximum flexion and extension of the spine, it is possible to determine the mobility or immobility of the intervertebral space.
The most modern and high-tech research methods are computed tomography (hereinafter referred to as CT) and magnetic resonance imaging (hereinafter referred to as MRI). Although the first CT and MRI machines appeared in the 70s and 80s, the technologies are still being actively developed and improved, while remaining quite inaccessible to the general population due to the high cost of examinations or the lack of machinesin local hospitals.
Methods of treatment of osteochondrosis of the spine
Treatment of osteochondrosis is a long and complex process. It aims to reduce and eliminate the consequences of changes in the intervertebral disc. Namely, inflammation, squeezing, poor blood flow, muscle spasms. Many types of therapy can help in this process, including the methods of oriental healers. In the treatment of osteochondrosis, the patient needs complete rest.
For the most part, the treatment is done with non-invasive methods, such as drug therapy, antiparasitic therapy, exercise therapy and others. Invasive therapy, that is, surgical operations, is rarely used. For example, in such cases when the intervertebral hernia continues for more than six months and conservative treatment does not give a positive effect.
Osteochondrosis of the spine and its treatment are performed by doctors of various specialties: a neurologist, an orthopedist, a vertebrologist, a chiropractor and others. However, the diagnosis, the appointment of analyzes and studies, is usually carried out by a neurologist, as well as a vertebrologist, if a doctor of such a specialty is available in the clinic, due to his specialization in diseases of the spine.
Summarizing, we can say that the treatment of osteochondrosis is divided into the following main categories:
- Reduction of pain syndrome;
- Removal of spasms;
- Elimination of inflammation;
- Reduction of squeezing;
- Improving blood circulation;
- Prevention of further deterioration.
Let's take a look at commonly used treatments, each of which covers one or more of the items on this list.
Physiotherapy treatment
Physiotherapy procedures are aimed at improving blood microcirculation in the area of the affected spine, eliminating pain and relieving edema. Also, physiotherapy helps to reduce the doses of drugs used. There are dozens of types of physical therapy. Here are some of them:
- Reflexology is the influence on acupuncture points with needles, current, laser. Helps relieve spasm and improve blood flow;
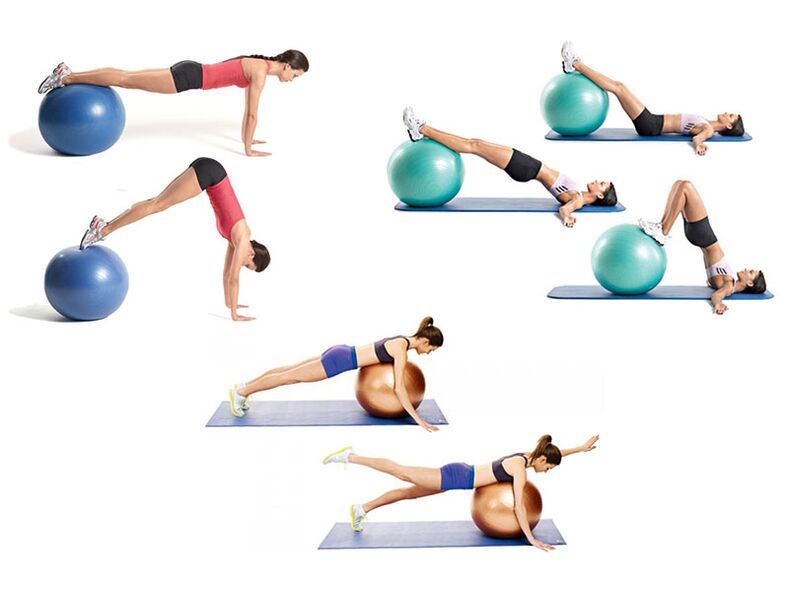
- Kinesitherapy is a treatment with movements and special physical exercises. In fact, this is therapeutic gymnastics, but in an expanded sense. This includes training in simulators, group exercises under the guidance of a doctor, stretching of the spine;
- Therapeutic swimming. Allows you to perform exercises with spinal cord injury for those patients who find it difficult to do them. For example, the elderly, people who are overweight or have limited motor skills. It is important to note that due to the lifting force of the water, there is a uniform distribution of loads on the back;
- Impulse current therapy, UHF therapy, neurostimulation, magnetotherapy, massage, etc.
Acupuncture
A unique method derived from oriental medicine. Its essence lies in the use of special very thin needles that enter specific points of the body, literally, under the influence of gravity. These points were discovered by thousands of years of experience of eastern healers, later confirmed by official medicine. Acupuncture helps to eliminate excruciating pains, has a positive effect on the nervous system as a whole and nervous diseases.
Surgical intervention
Surgery is indicated only if there is no positive effect from non-invasive treatment or in case of severe complications. The main method of surgical treatment is discectomy - removal of a damaged disc. However, even after surgery using minimally invasive methods, rehabilitation will take at least 6 months.
At the same time, the operation will not eliminate the need for regular treatment of osteochondrosis. Since before the operation there is always a clear task to eliminate a specific defect: hernia, deformation, subluxation, etc. The operation does not affect the general process of degeneration of the cartilage tissue of the spine.
Medical treatment
This type of treatment is more effective in the short term. Medicines immediately reduce pain, eliminate inflammation, relieve spasms, etc. However, as soon as they are canceled, in the absence of other procedures necessary for the treatment of osteochondrosis, their effect will quickly disappear. At the same time, you cannot spend your whole life on drugs, sooner or later they will have a side effect on the body.

Medications can be classified as primary and secondary treatment. They are often necessary to improve the patient's life. They are used to relieve pain (therapeutic blockade), eliminate inflammation, relieve muscle spasms, improve blood flow. In recent years, another type of drug is increasingly being used - chondroprotectors. However, medicines alone cannot achieve a permanent long-term effect.
Treatment at home
Home treatment of osteochondrosis consists of manual therapy (exercise therapy, Shants collar), acupuncture and vacuum therapy. These methods help improve blood circulation and reduce strain on the muscles and back. As a result, tissue regeneration is significantly improved.
The listed procedures in combination with medicines provide an effective treatment that relieves unpleasant symptoms and improves the general condition. In this case, special attention should be paid to proper nutrition and regulation of excess weight.
Physiotherapy
Thanks to gymnastics, the mobility of the vertebrae is restored, their muscles and blood circulation system are strengthened. The latter is of great importance, because the spine is deprived of the blood supply system and the intervertebral disc can receive nutrients only through the adjacent tissues. In this case, it is necessary to distinguish between therapeutic exercises and any other training.

Manual therapy
One of the most effective methods. Since the manual therapist touches the muscles, ligaments and bones. Improves posture, restores the "normal" structure of the skeleton, relieves excessive muscle tension. Including, it directly affects the vertebrae.
Manual therapy of osteochondrosis should be carried out regularly, from once a year to several, depending on the need. It should be noted that this is not a one-time, multidimensional procedure lasting 10-20 sessions. Only then will there be a long-term positive effect.

























